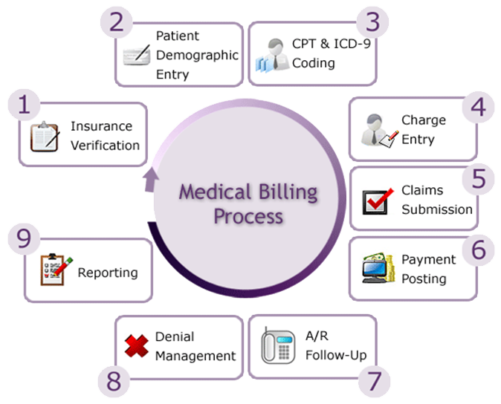
Medical Billing - What we do ??
We are one of the leading medical billing outsourcing company offering high quality services to our clients. Our current information Databases helps us perform greater in-depth analysis and research, which in turn translate to accuracy and reliability in medical claims management. We have experience with most of the popular billing software applications.
We use HIPAA compliant VPN (Virtual Private Networks) to access your systems. Our staff will perform the medical billing functions on your systems, exactly the way they used to be done, the only difference being that they would be physically in our facility. This means that all your processes and reports remain exactly the same.
Demographics & Charges
We have well qualified staffs to enter the PT demographics and Charges which has been received from the provider, Work has been done within the TAT to avoid claims late submissions and reduce the denials from payer, More than work audit is done on the same day before billing the claim to insurance and Eligibility is verified every time before billing a claim.
Payment Posting
Payment posting has been done in two ways by Manual and ERA. If denials found in ERA they are done by manual by obtaining EOB to avoid incorrect denial posting and valid EOB to AR process to resolve the denial easily. Payment is posted with High accuracy as per EOB and payment reports will be updated to clients in daily bases.
Accounts Receivable
We understand the importance of accurately and quickly processing your claims so that it will help you to maximize your revenue and improve your cash flow. Priority is given to old aged claims to reduce balance adjustments. AR actions can be done on a daily basis and assistance from client to increase in collection ratio through accurate analysis and timely followup. Old AR mare also analyzed and corrective measures will be taken.
PT Statements
Patient statements have been done twice in a month based on client instructions and requirement. Level of Patient has been set to obtain from patient without moving them to collections.
Medical Coding
CrescereMed takes pride in providing timely and accurate coding services to hospitals and physician practices. We have proven track record of minimizing denials while improving coding quality and compliance for our clients. Our coding team has AAPC certified coders with in-depth understanding of latest coding regulations of patient care in hospital and clinical settings. Our qualified expert team reviews physician and hospital records and assess accuracy of available documentation in ER records in comparison to descriptions of assigned Current Procedural Terminology (CPT) codes provided by the Center for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA).
Service Types & Specialities
Inpatient Surgery
Outpatient Surgery
Evaluation & Management
Internal Medicine
Dermatology
Resources:
Our coding staffs have received extensive training under coding experts. Certified coders monitor their work regularly and external coding and compliance experts periodically audit the coding department. Our coders are proficient with:
- PT, ICD-10, and HCPCS coding across various specialties.
- Payer-specific coding requirements.
- Insurance and governmental regulatory requirements.
- Software like ENCODERPRO, Supercoder.